The Silent Threat: Understanding Antibiotic Resistance
Published on December 25, 2025 by Admin

Antibiotics have revolutionized medicine. They are powerful tools that save lives. However, a growing crisis threatens their effectiveness. This is antibiotic resistance. It is a silent pandemic. It affects everyone, from public health advocates to parents and medical students.
Understanding this threat is crucial. We must act now to preserve these life-saving drugs. This article will explore the causes, impacts, and potential solutions to antibiotic resistance.
What is Antibiotic Resistance?
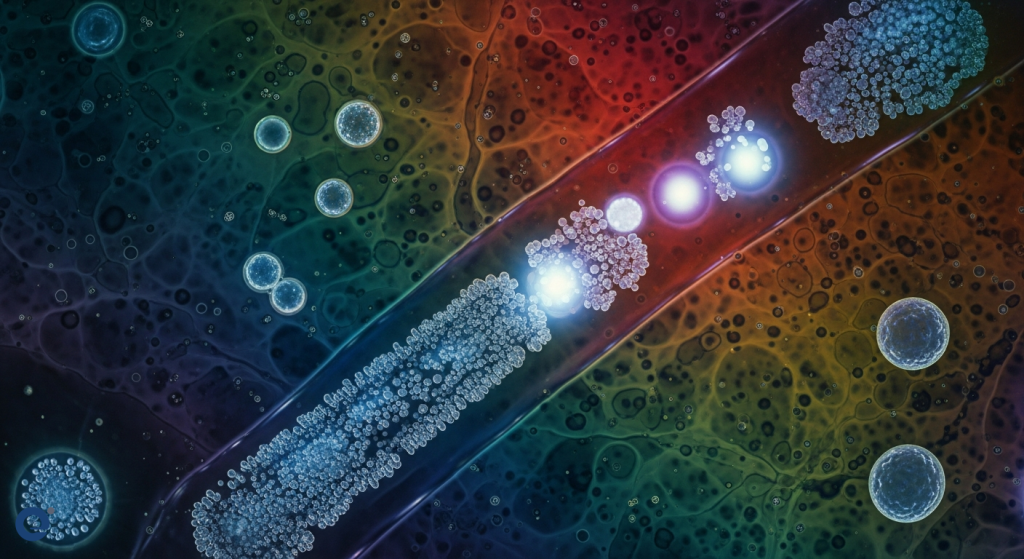
Antibiotic resistance occurs when bacteria change. These changes make them resistant to antibiotics. Antibiotics are medicines that kill or slow the growth of bacteria. When bacteria become resistant, antibiotics no longer work. This makes infections harder to treat.
Essentially, the microbes evolve. They develop structural and functional modifications. These include reduced drug permeability. They also increase efflux pumps. Furthermore, bacteria can modify antibiotics enzymatically. They can also change their drug targets. Intracellular infections and biofilm creation are other mechanisms.
The Growing Crisis: Why Now?
Antibiotic resistance is not new. However, it has accelerated alarmingly. Several factors contribute to this crisis. Overuse and misuse of antibiotics are primary drivers. This happens in both human medicine and agriculture.
Moreover, there’s a lack of new antibiotics under development. The healthcare industry’s focus on profit can also play a role. The absence of diagnostic testing before prescribing antibiotics is another issue. This leads to unnecessary prescriptions.
Key Drivers of Resistance
The global spread of antibiotic resistance is driven by multiple factors. Overuse in livestock is a major contributor. Animals are often given antibiotics for growth promotion and feed efficiency. This creates a breeding ground for resistant bacteria.
Other factors include:
- Drug efficacy issues.
- Development of fewer new vaccines.
- Environmental toxicity from antibiotic residues.
- Transmission through travel and trade.
- Lack of funding for healthcare research and development.
The COVID-19 pandemic also saw an increase in resistance. This was due to improper prescriptions. Cancer patients are also at higher risk. This is because their immune systems are often weakened.
How Resistance Develops and Spreads
Antibiotic resistance develops through evolutionary processes. Mutations can occur naturally in bacteria. These mutations can confer resistance. However, the spread of resistance is more complex. It often involves the transmission of already resistant bacteria.
Dr. Lance Price explains that we often carry low levels of drug-resistant bacteria. We pick them up from various sources, like the food supply. These resistant strains can live in our guts or noses without causing symptoms. They are opportunistic pathogens.
When we take antibiotics, they kill the susceptible bacteria. This creates an advantage for the resistant strains. They can then thrive and out-compete the others. As a result, we end up with a higher concentration of resistant bacteria in our bodies.
It’s important to remember that we are walking ecosystems. Our bodies host a complex microbiome. Diverse bacterial communities are usually a sign of health. However, when resistant bacteria colonize us, they can cause problems later.
The transmission of these resistant bacteria is common. This can happen silently. It occurs both within and outside healthcare facilities. This human-to-human interface is a primary route for AMR spread. The unrestricted use of antimicrobials in livestock feed has also been a major contributing factor.
The Impact of Antibiotic Resistance
The consequences of antibiotic resistance are severe. Infections caused by resistant bacteria are harder to treat. This leads to longer illnesses. It also results in significant morbidity and mortality. The financial impact is also substantial.
Modern medical procedures rely heavily on antibiotics. Surgeries, chemotherapy, and organ transplants would become far riskier without effective antibiotics. A world without effective antibiotics would be a world where common infections could kill again.
The World Health Organization calls antibiotic resistance an existential threat to humanity. In 2019 alone, drug-resistant germs and bugs killed 5 million people. This number is projected to rise if we do not act.
What Can Be Done? Solutions and Interventions
Addressing antibiotic resistance requires a multi-faceted approach. It demands urgent intervention at local, national, and global levels. Several strategies are being explored and implemented.
Minimizing Overuse and Misuse
A crucial step is to minimize the overuse of antibiotics. This applies to both human medicine and agriculture. Over-the-counter antibiotics should be strictly regulated. Antibiotics should not be used routinely in food animals for growth promotion.
Diagnostic testing is essential. Doctors should use rapid diagnostic tests before prescribing antibiotics. This helps ensure that antibiotics are used only when truly necessary and for the correct pathogen.
Developing New Therapies
There is a critical need for new antibiotics. However, the discovery and development of novel antimicrobial drugs have slowed. This is partly due to economic challenges. The return on investment for new antibiotics is often lower than for other drugs. This paucity in discovery stands in sharp contrast to demand.
However, modern therapeutic alternatives are being developed. These include:
- Nanoparticle-based approaches.
- Bacteriophage therapy.
- Antimicrobial biochemical approaches.
These alternatives offer hope for curbing widespread resistance.
Surveillance and Monitoring
Effective surveillance and monitoring systems are vital. These systems help track the emergence and spread of resistant bacteria. This data is crucial for informing public health policies and interventions. Understanding the prevalence of antimicrobial-resistant bacteria worldwide is key.
Access to quality and affordable medicines, vaccines, and diagnostics is also important. Furthermore, enforcement of legislation related to antibiotic use is necessary.
The One Health Approach
A holistic approach, known as “One Health,” is essential. This recognizes the interconnectedness of human, animal, and environmental health. It emphasizes collaborative action across sectors.
This coordinated effort requires collaboration among multiple national and international organizations. Without such orchestrated action, a post-antibiotic era could become a stark reality.
What causes antibiotic resistance? – Kevin Wu
The Role of Public Health Advocates, Parents, and Medical Students
Each group has a vital role to play in combating antibiotic resistance.
Public Health Advocates
Advocates can raise public awareness. They can lobby for stronger policies. They can also push for increased funding for research and development. Educating communities about the responsible use of antibiotics is paramount.
Parents
Parents are key in ensuring children receive antibiotics only when prescribed by a doctor. They should understand that antibiotics are not effective against viruses like the common cold. Following a doctor’s instructions for completing the full course of antibiotics is also crucial, even if the child feels better.
Medical Students
Medical students are the future healthcare providers. They must be thoroughly educated on antimicrobial stewardship. This includes understanding when to prescribe antibiotics, choosing the right drug, and educating patients. Their commitment to evidence-based prescribing will shape the future of antibiotic use.
Conclusion: A Call to Action
Antibiotic resistance is a serious and growing global threat. It is a silent pandemic that requires our immediate attention. The overuse and misuse of antibiotics, coupled with a lack of new drug development, have accelerated this crisis. The consequences are dire, threatening modern medicine and global health.
However, solutions exist. By minimizing overuse, developing new therapies, enhancing surveillance, and adopting a One Health approach, we can fight back. Public health advocates, parents, and medical students all have critical roles to fulfill.
It is high time to explore new alternatives. We must curtail the enormous increase in resistant pathogens. This is essential to prevent an incurable global confrontation. Let us work together to save antibiotics for future generations.
Frequently Asked Questions
What is the most common way antibiotic resistance spreads?
The most common way antibiotic resistance spreads is through the transmission of already resistant bacteria between people, both in healthcare settings and in the community.
Are antibiotics effective against viruses?
No, antibiotics are not effective against viruses. They only work against bacteria. Using antibiotics for viral infections contributes to antibiotic resistance.
What is the “One Health” approach?
The “One Health” approach recognizes that human health, animal health, and environmental health are interconnected. It promotes collaboration across these sectors to address complex health challenges like antibiotic resistance.
Why is there a lack of new antibiotics being developed?
Developing new antibiotics is scientifically challenging and costly. Furthermore, the economic incentives for pharmaceutical companies are often lower compared to drugs for chronic conditions, as antibiotics are typically used for short durations.
How can I protect myself from antibiotic-resistant infections?
You can protect yourself by practicing good hygiene, such as frequent handwashing. Ensure you only take antibiotics when prescribed by a healthcare professional and complete the full course as directed. Also, be mindful of food safety practices, especially regarding meat and poultry.

