Fascia’s Vital Role: Unlocking Connective Tissue Health
Published on December 31, 2025 by Admin

Fascia, often overlooked, is a crucial connective tissue that plays a significant role in our body’s structure and function. Understanding its importance is key for physical therapists, athletes, and yoga practitioners aiming to improve mobility and reduce pain.
The Fascia: Your Body’s Unsung Hero
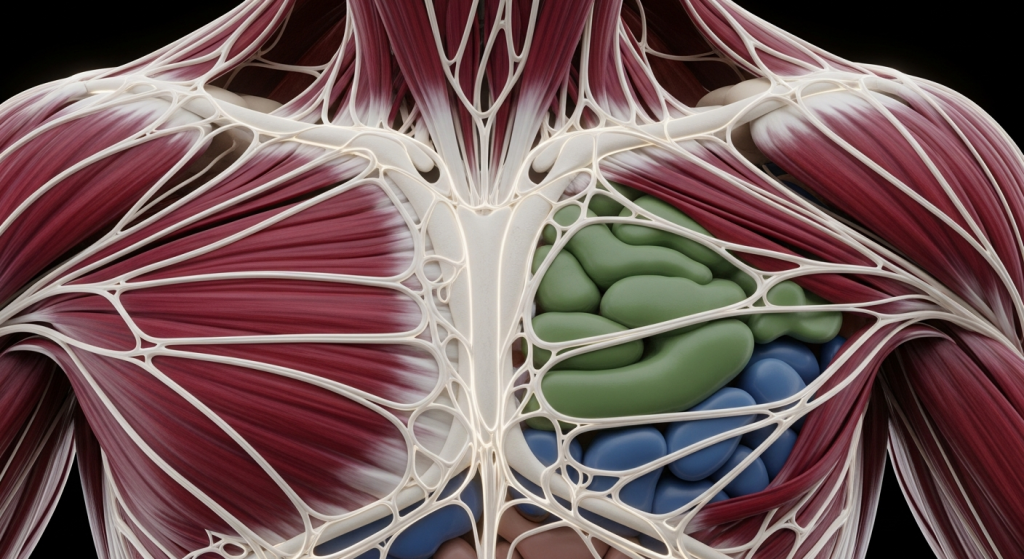
Fascia is a thin, stringy, and fibrous connective tissue that envelops and supports nearly every structure within your body. Think of it as a continuous, three-dimensional web that surrounds your muscles, tendons, ligaments, organs, nerves, joints, and bones. Initially, scientists believed fascia’s primary role was simply to provide support. However, recent discoveries reveal it’s much more complex, acting as a system-wide network that dictates form and function throughout your entire body.
This remarkable tissue is primarily composed of collagen, a protein that gives it both strength and flexibility. Fascia is typically soft and loose, existing in multiple layers. Between these layers is a liquid called hyaluronan. This substance acts as a lubricant, allowing your fascia to stretch and slide smoothly as you move. When this hyaluronan dries up due to inflammation or trauma, the fascial layers can tighten, restricting movement and leading to pain.
What Does Fascia Actually Do?
Fascia’s functions are diverse and essential for optimal bodily performance. Firstly, it provides crucial structure and support. It holds your muscles together, enabling them to contract and stretch effectively. Moreover, fascia creates a smooth gliding surface for your muscles, joints, and organs, preventing friction and potential tears during movement.
Additionally, fascia stabilizes your body structures, contributing significantly to overall strength. It separates individual muscles, which helps to ease muscle tension. This separation also aids in joint stability and smooth movement. Furthermore, healthy fascia can improve circulation throughout the body, ensuring all systems work harmoniously together. It essentially provides the environment where all your body systems can function optimally.
Understanding the Layers of Fascia
Fascia isn’t a single, uniform layer. Instead, it’s organized into four distinct layers, each with a specific location and role:
- Superficial Fascia: This is the outermost layer, situated directly beneath your skin. It’s composed of loosely packed collagen and elastic fibers and is thicker in areas like the chest and back, becoming thinner in the arms and legs.
- Deep Fascia: This layer surrounds your entire musculoskeletal system. It encases muscles, bones, tendons, cartilage, nerves, and blood vessels. Deep fascia is generally thicker than superficial fascia and has two subtypes:
- Aponeurotic Fascia: This is thick, pearly-white tissue that separates more easily from muscles.
- Epimysial Fascia: This subtype is thinner and more tightly connected to the muscles it surrounds.
- Visceral Fascia: This layer encapsulates the organs within your abdomen, as well as your lungs and heart.
- Parietal Fascia: This fascia lines the walls of specific body cavities, such as the pelvic region.
The Difference Between Fascia, Tendons, and Ligaments
While all three are made primarily of collagen, their locations and functions differ. Tendons connect muscles to bones, allowing for movement when muscles contract. Ligaments, on the other hand, connect bones to other bones, providing joint stability. Fascia, however, wraps around muscles and other body parts, forming a continuous network that supports and separates these structures. Examples include the thoracolumbar fascia in the back, fascia lata in the thigh, and plantar fascia in the foot.
When Fascia Tightens: Conditions and Disorders
When fascia is healthy, it remains relaxed and flexible, stretching with your body’s movements. However, factors like inflammation, trauma, or prolonged poor posture can lead to the drying up of hyaluronan. Consequently, the fascial layers can tighten around muscles and other tissues. This restriction can manifest as pain and limited mobility.
Many conditions and disorders can affect fascia. For instance, muscle pain can sometimes stem from fascial issues rather than muscle damage alone. When fascia becomes restricted, it can impede the normal gliding of muscles and tissues, leading to discomfort and compensatory movement patterns.
Patients experiencing connective tissue hyper- or hypo-mobility disorders often suffer from musculoskeletal pain. Many also exhibit abnormal proprioception, which is the body’s sense of its position in space. The intricate relationships among fascia mobility, proprioception, and myofascial pain are areas of ongoing research, but a better understanding could significantly improve care for those with chronic pain.
The Crucial Role of Fascia Mobility
Fascia mobility, particularly along the shear planes that separate muscles, is vital for proper musculoskeletal function. This mobility allows for smooth, unimpeded movement between different tissue layers. When these fascial planes become adhered, perhaps due to scarring from an injury or chronic postural habits, interfacial mobility is lost. The consequences of reduced fascia mobility can be profound, affecting the function of muscles and joints in ways that are still being fully understood.
Furthermore, fascia is surprisingly rich in nerve endings. These small diameter fibers can transmit nociceptive signals, especially when inflammation is present. This means that fascial restrictions can directly contribute to pain perception. The sensory information derived from fascia also plays a role in proprioception, our internal “body-sense.” This aspect is crucial for coordinated movement and balance.
Fascia’s Connection to Proprioception and Pain
Proprioception is our brain’s awareness of our body’s position, movement, and balance. Fascia, with its extensive network of sensory receptors, is a key player in this process. It provides constant feedback to the nervous system about the body’s state. When fascia is restricted or dysfunctional, this feedback can become inaccurate, leading to impaired coordination and an increased risk of injury.
The clinical syndrome of “myofascial pain” is estimated to affect a significant portion of individuals with chronic musculoskeletal pain. This pain often occurs in the back, neck, shoulders, hips, and pelvis. It can also be associated with temporomandibular joint pain and headaches. The underlying mechanisms are complex, but restricted fascia and its impact on nerve signaling are strongly implicated.
Enhancing Fascia Health Through Movement and Therapy
Maintaining healthy, flexible fascia is paramount for overall well-being and physical performance. Fortunately, connective tissue issues are often addressable through conservative, non-invasive care. Both physical therapists and practitioners of other movement modalities can significantly impact fascial health.
The Power of Movement
Regular movement is one of the most effective ways to support fascia health. It keeps tissues pliable and helps maintain a full range of motion. Whether through walking, stretching, or daily activities, moving your body encourages healthy, supple fascia. Dynamic stretches, in particular, can improve mobility and help prevent tightness in connective tissues.
For athletes and active individuals, robust connective tissues are essential for efficient force transfer and injury prevention. Strength is largely dependent on the quality and quantity of these dense connective tissues. More robustness leads to more efficient energy transfer from muscular contraction to body action.
Therapeutic Interventions for Fascia
Physical therapists often employ various techniques to address fascial restrictions. These can include:
- Myofascial Release (MFR): This technique involves applying gentle, sustained pressure to fascial restrictions. The goal is to release tension and restore mobility. MFR can help calm the nervous system and improve circulation.
- Deep Tissue Massage: This approach uses firm pressure to reach deeper layers of muscle and surrounding connective tissue. It’s particularly helpful for easing long-standing tension and stiffness.
- Stretching and Mobility Exercises: Targeted exercises can help lengthen and mobilize fascial tissues.
Research suggests that techniques like myofascial release can improve the flexibility of tissues like the plantar fascia, especially in individuals with conditions like plantar fasciitis. The gentle, sustained pressure helps to stretch and release tight connective tissue.
The Role of Massage Therapy
Massage therapy, especially techniques like myofascial release, is believed to significantly impact fascial mobility. By manually stretching and manipulating the fascia, massage can potentially relieve tension and improve overall movement. One of the underlying mechanisms involves collagen remodeling. Mechanical pressure, such as that applied during massage, can stimulate collagen remodeling, enhancing tissue elasticity and function.
Regular massage therapy shows promise in improving connective tissue flexibility, offering benefits for mobility and injury prevention. However, more research is continually needed to fully understand the mechanisms involved and to establish optimal techniques.
Collagen Production and Fascial Strength
Recent research highlights the importance of specific mechanical stresses for maximizing new collagen cell production. When collagen cells are subjected to moderate, sustained stress, they release chemical signals that stimulate the production of new cells, leading to a more robust matrix. For tendon and fascia, this can be achieved through performing four 30-second moderately vigorous isometric contractions with a two-minute recovery interval, repeated within a ten-minute window every six hours. This targeted approach can enhance the resilience of dense connective tissue.
Maintaining Fascia Health: Practical Tips
While professional therapies are beneficial, consistent self-care is also vital for maintaining fascia health. Here are some practical tips:
- Stay Hydrated: Water is essential for keeping fascia flexible and resilient. Proper hydration reduces stiffness and discomfort.
- Move Regularly: Consistent movement, including dynamic stretching, keeps tissues pliable and supports a full range of motion.
- Self-Massage Techniques: Using tools like foam rollers or massage balls can help release tension in specific areas. Be gentle but consistent.
- Mindful Posture: Pay attention to your posture throughout the day. Prolonged poor posture can lead to fascial restrictions. You can learn more about correcting poor posture with simple exercises.
Frequently Asked Questions about Fascia
What is fascia and why is it important?
Fascia is a connective tissue that surrounds and supports all structures in your body. It’s crucial for structural integrity, facilitating movement, and providing support for muscles, organs, and bones. Healthy fascia is flexible and allows for smooth gliding between tissues.
Can tight fascia cause pain?
Yes, when fascia becomes tight or restricted, it can restrict the movement of muscles and tissues, leading to pain and discomfort. This is often referred to as myofascial pain.
How can I improve my fascia mobility?
You can improve fascia mobility through regular movement, dynamic stretching, staying hydrated, and employing self-massage techniques like foam rolling. Professional therapies like myofascial release and deep tissue massage are also highly effective.
What is the difference between fascia, tendons, and ligaments?
Tendons connect muscles to bones, ligaments connect bones to bones, and fascia is a broader connective tissue that wraps around and supports muscles, organs, nerves, and other structures, forming an interconnected network throughout the body.
Are there different types of fascia?
Yes, there are four main layers: superficial, deep, visceral, and parietal fascia, each serving distinct roles in supporting different parts of the body.
Conclusion: Prioritizing Fascial Health for Optimal Function
Fascia is an indispensable component of our musculoskeletal system, deeply influencing our mobility, performance, and overall health. By understanding its structure and function, and by incorporating practices that promote its health, individuals can significantly reduce pain, enhance movement quality, and improve their athletic or yogic performance. Whether you are a physical therapist guiding patients, an athlete striving for peak performance, or a yoga practitioner deepening your practice, recognizing and addressing fascial health is a fundamental step towards a more resilient and capable body.

