Antibiotic Resistance: The Global Threat and New Treatments
Published on January 12, 2026 by Admin

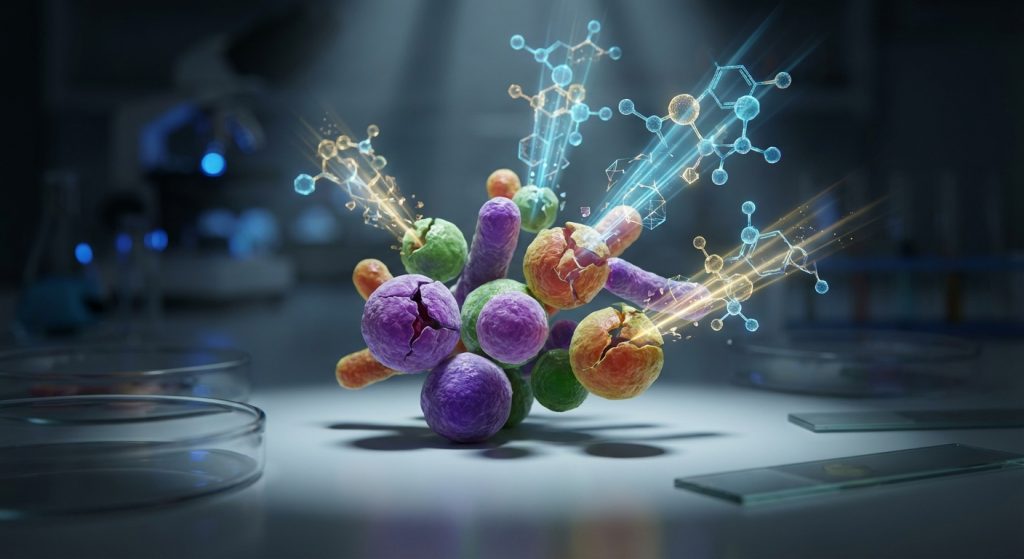
Antibiotic resistance is a major global health crisis. It makes infections harder to treat. This is a serious concern for everyone. Pharmacologists, researchers, and public safety advocates are working hard. They are trying to find new ways to fight this threat.
Understanding the Growing Crisis
Antibiotics are powerful medicines. They save millions of lives each year. However, bacteria can adapt and change. They become resistant to these drugs. This means antibiotics stop working. Infections then become very difficult to cure. This is known as antimicrobial resistance (AMR).
The problem is growing rapidly. Overuse and misuse of antibiotics are key drivers. This happens in both human medicine and agriculture. When antibiotics are used too often, bacteria are exposed. They have more chances to develop resistance. Therefore, responsible use is crucial.
Furthermore, poor infection control contributes to AMR. This is especially true in healthcare settings. Hospitals can become breeding grounds for resistant bacteria. Strict hygiene measures are essential. They help prevent the spread of infections.
The Impact on Public Health
Antibiotic resistance poses a significant threat to public health. Common infections can become deadly again. Procedures like surgery and chemotherapy become riskier. They rely on effective antibiotics to prevent infections.
The economic burden is also substantial. Treating resistant infections costs more. It requires longer hospital stays. It also leads to lost productivity. This strains healthcare systems worldwide. In conclusion, AMR impacts individuals and economies.
For example, drug-resistant tuberculosis is a major challenge. It is harder to treat and requires longer therapy. Similarly, resistant strains of E. coli and Salmonella cause severe foodborne illnesses. The consequences are far-reaching.
The Race for New Treatments
The development of new antibiotics is a race against time. However, creating new drugs is complex. It is also very expensive. Pharmaceutical companies have invested less in antibiotic research. This is partly due to economic reasons. New antibiotics are typically used sparingly. This limits their market potential.
Researchers are exploring various avenues. They are looking for novel drug targets. They are also investigating alternative therapies. These include phage therapy and immunotherapy. These approaches offer promise. However, they require extensive research and development.
Moreover, understanding bacterial mechanisms is vital. Scientists are studying how resistance develops. This knowledge helps in designing new drugs. It also informs strategies to overcome resistance. Therefore, a multi-pronged approach is necessary.
Innovative Drug Discovery
New antibiotics are being discovered. Some are derived from natural sources. Others are created through synthetic biology. Scientists are using advanced techniques. They are screening vast libraries of compounds. They are also using AI to predict potential drug candidates. This accelerates the discovery process.
For instance, researchers are looking for compounds that can disarm bacteria. Instead of killing them directly, these compounds might make them vulnerable. This could reduce the pressure for resistance to develop. As a result, this strategy might prolong the effectiveness of existing drugs.
Beyond Traditional Antibiotics
Alternative treatments are gaining traction. Phage therapy uses viruses that infect and kill bacteria. This is a natural approach. It has shown success in treating resistant infections. However, regulatory hurdles exist.
Immunotherapy is another promising area. This involves boosting the patient’s own immune system. It helps the body fight off infections. This approach can be highly specific. It targets the bacteria without harming beneficial microbes.
Furthermore, combination therapies are being explored. Using multiple drugs or approaches together can be effective. It makes it harder for bacteria to develop resistance to all treatments simultaneously. This is a critical strategy for managing complex infections.
The Role of Public Health and Policy
Addressing antibiotic resistance requires global cooperation. Public health initiatives play a key role. These include promoting responsible antibiotic use. They also focus on improving hygiene and sanitation.
Governments and international organizations are implementing policies. These policies aim to incentivize antibiotic research. They also promote stewardship programs. These programs encourage healthcare providers to prescribe antibiotics judiciously.
Public awareness campaigns are also important. Educating the public about AMR helps. It encourages responsible behavior. People need to understand when antibiotics are necessary. They also need to know the risks of misuse.
The concept of One Health is highly relevant here. It recognizes the interconnectedness of human, animal, and environmental health. Tackling AMR effectively requires a holistic approach that considers all these aspects.
Challenges and Future Directions
Despite ongoing efforts, significant challenges remain. The pipeline for new antibiotics is still thin. Developing effective vaccines against bacterial infections is also difficult.
Moreover, resistance can spread rapidly across borders. This necessitates international collaboration. Sharing data and best practices is essential. We need to monitor resistance patterns globally. This helps in identifying emerging threats early.
The future of combating AMR lies in innovation. It also lies in sustained commitment. We need continued investment in research and development. Furthermore, we need strong political will to implement effective policies.
Key Strategies for Combating AMR
- Promote responsible antibiotic use in human and animal health.
- Strengthen infection prevention and control measures in healthcare settings.
- Invest in research and development of new antibiotics and alternative therapies.
- Enhance global surveillance of antibiotic resistance patterns.
- Educate the public about the risks of antibiotic resistance.
- Foster international collaboration and policy implementation.
Finally, adopting a One Health approach is paramount. This integrated strategy recognizes that the health of people is closely connected to the health of animals and our shared environment. By understanding these connections, we can develop more effective and sustainable solutions to combat AMR.
Frequently Asked Questions
What is antibiotic resistance?
Antibiotic resistance occurs when bacteria change. They evolve to resist the effects of antibiotics. This makes infections harder to treat.
Why is antibiotic resistance a global threat?
It makes common infections life-threatening. It increases healthcare costs. It also makes medical procedures riskier. Furthermore, it can lead to outbreaks that spread globally.
What causes antibiotic resistance?
The main causes are the overuse and misuse of antibiotics. This includes not finishing a full course of antibiotics. It also includes using antibiotics for viral infections, which they cannot treat.
What are some new treatments being developed?
Researchers are developing new antibiotics. They are also exploring phage therapy, immunotherapy, and combination therapies. These aim to overcome or bypass resistance mechanisms.
How can I help prevent antibiotic resistance?
Only take antibiotics when prescribed by a doctor. Complete the full course as directed. Do not share antibiotics with others. Practice good hygiene to prevent infections.

